Lymphedema is a chronic and often progressive medical condition characterized by the accumulation of lymphatic fluid, leading to swelling, typically in one or more extremities. This condition can have a significant impact on a person’s quality of life, and understanding its causes and management is crucial. In this comprehensive article, we will explore lymphedema, its underlying mechanisms, its causes, and the various strategies for prevention and treatment.
Understanding Lymphedema
Before delving into its causes, let’s establish a foundational understanding of lymphedema:
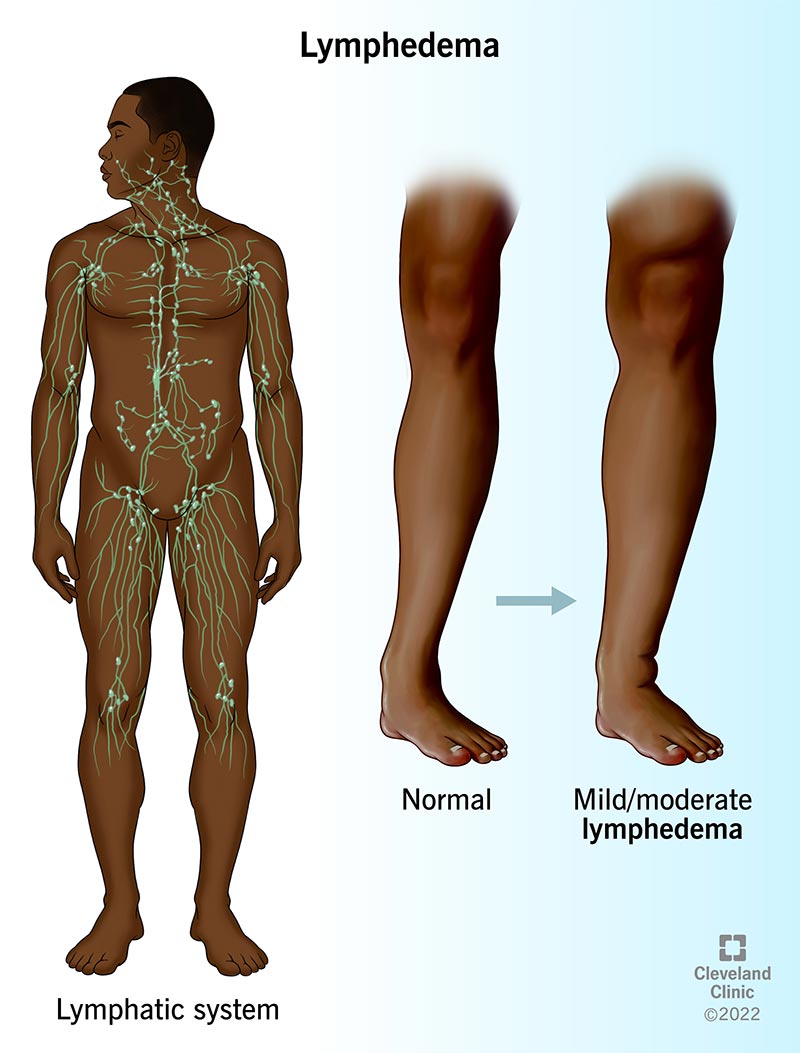
The Lymphatic System
The lymphatic system is a vital component of the circulatory and immune systems. It consists of a network of lymphatic vessels, lymph nodes, and lymphatic organs such as the spleen and thymus. The primary function of the lymphatic system is to transport lymph, a clear fluid containing white blood cells and waste products, back into the bloodstream, while also playing a crucial role in immune defense.
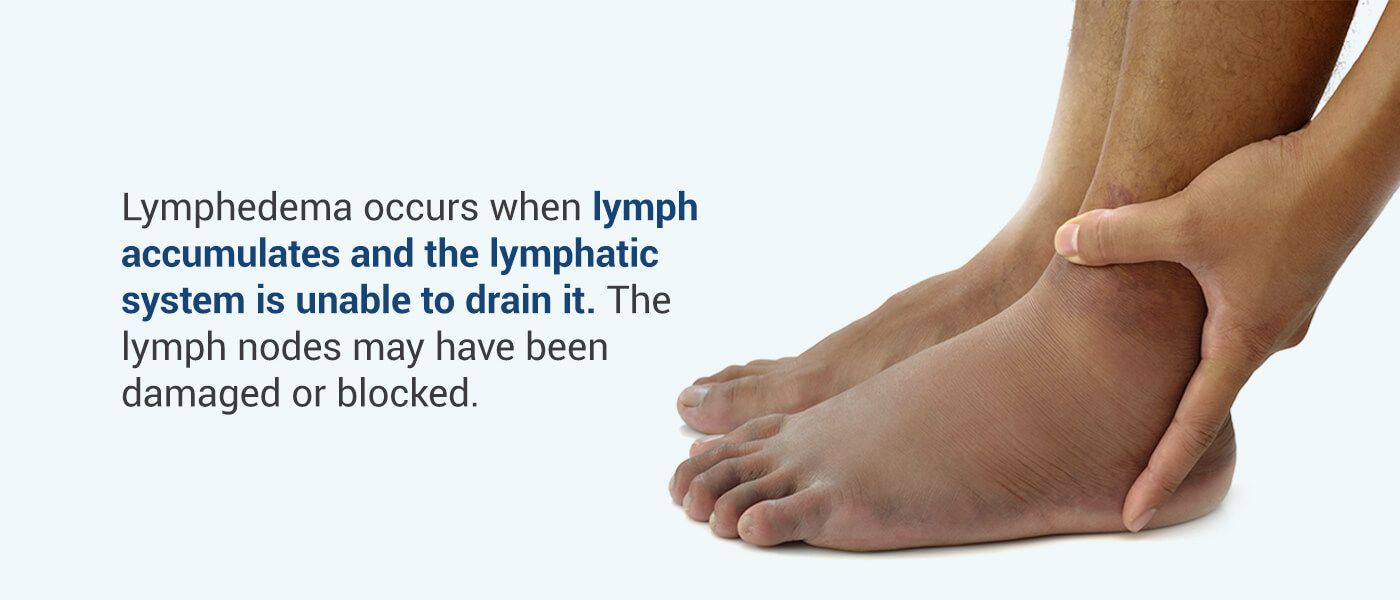
Lymphedema Defined
Lymphedema occurs when the normal flow of lymph is obstructed or impaired, leading to the accumulation of lymphatic fluid in the affected area. This results in chronic swelling, discomfort, and potential complications. There are two primary types of lymphedema:
- Primary Lymphedema: This type is typically present at birth or develops later in life due to a congenital abnormality or genetic predisposition. Primary lymphedema is less common and often occurs without an identifiable cause.
- Secondary Lymphedema: Secondary lymphedema is the more common form and is typically the result of damage or disruption to the lymphatic system due to surgery, radiation therapy, infection, trauma, or cancer. It can develop days, months, or even years after the initial injury or insult.
Causes of Lymphedema
Lymphedema can be caused by various factors, often related to an interruption of the normal lymphatic flow:
1. Cancer and Cancer Treatment:
- Surgery: Lymph nodes may be removed during cancer surgery, leading to impaired lymphatic drainage. Common surgeries include mastectomy for breast cancer and lymph node dissection for melanoma.
- Radiation Therapy: Radiation can damage lymphatic vessels, scarring them and reducing their ability to transport lymph.
2. Infection:
Infections such as cellulitis or filariasis can damage lymphatic vessels and lead to the development of lymphedema, especially in regions where these infections are prevalent.
3. Trauma:
Physical injury, burns, or severe tissue damage can disrupt lymphatic vessels and cause lymphedema.
4. Obesity:
Excess body weight can place pressure on the lymphatic system, impeding the flow of lymph and contributing to the development of lymphedema.
5. Inflammatory Conditions:
Chronic inflammatory conditions like rheumatoid arthritis or systemic lupus erythematosus can result in inflammation of lymphatic vessels.
6. Congenital Factors:
Rare genetic disorders, such as Milroy disease and hereditary lymphedema, can cause primary lymphedema.
7. Surgical Procedures:
Even surgeries unrelated to cancer can accidentally damage lymphatic vessels, leading to secondary lymphedema.
Signs and Symptoms of Lymphedema
Lymphedema typically presents with the following signs and symptoms:
- Swelling: Persistent swelling, often in an arm or leg, but it can affect other body parts as well.
- Heaviness: A feeling of heaviness or tightness in the affected limb.
- Limited Range of Motion: Reduced flexibility and mobility in the affected area.
- Recurring Infections: Frequent skin infections due to the compromised immune function in the affected limb.
- Hardened Skin: Thickening and hardening of the skin, known as fibrosis, which can make the limb less pliable.
Prevention and Management
While lymphedema is a chronic condition, several strategies can help prevent its development and manage its symptoms:
1. Education:
Patients at risk of lymphedema, such as those who have had cancer surgery or radiation, should receive education on the importance of proper limb care and early detection.
2. Compression Garments:
Wearing compression garments, such as sleeves or stockings, can help maintain lymphatic flow and reduce swelling.
3. Physical Therapy:
Specially trained physical therapists can provide exercises and techniques to stimulate lymphatic drainage and improve mobility.
4. Manual Lymphatic Drainage (MLD):
This specialized massage therapy can help move lymphatic fluid from the swollen area to regions with healthy lymphatic flow.
5. Complete Decongestive Therapy (CDT):
CDT combines MLD with compression therapy, exercise, and skin care to manage lymphedema effectively.
6. Surgery:
In severe cases, surgical interventions like lymphatic bypass or lymph node transfer may be considered.
Conclusion
Lymphedema is a complex and often life-altering condition that can result from various underlying causes. It is essential for individuals at risk, particularly cancer survivors, to be vigilant about early detection and management. With proper education, preventative measures, and therapeutic interventions, individuals with lymphedema can effectively manage their condition, reduce symptoms, and improve their overall quality of life. Advances in research and treatment options continue to offer hope for those affected by this challenging condition, highlighting the importance of ongoing medical research and patient support.