How do the Kidneys Filter Waste from the Blood: The Marvelous Mechanism of Renal Filtration
The kidneys are remarkable organs, performing a vital role in maintaining the body’s internal balance by filtering waste and excess substances from the bloodstream. This process, known as renal filtration, is a complex and highly efficient system that ensures the removal of harmful waste products while preserving essential nutrients and electrolytes. In this comprehensive article, we will delve into the intricate world of renal filtration, exploring its anatomy, mechanisms, regulation, and the pivotal role it plays in overall health.
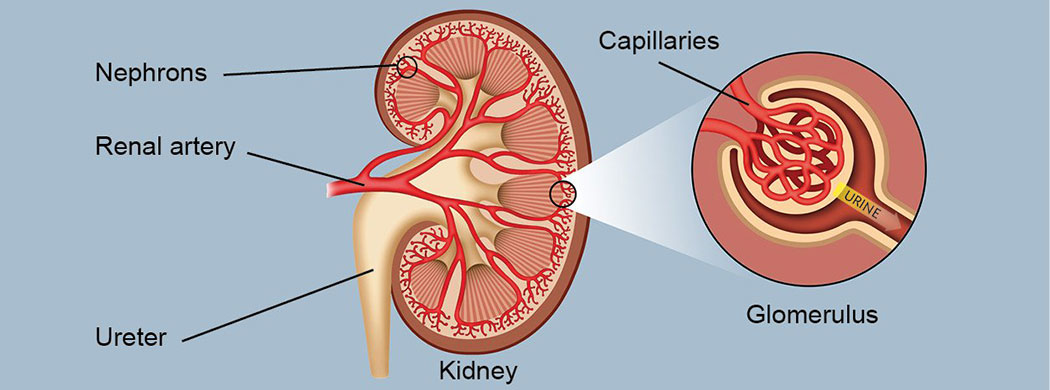
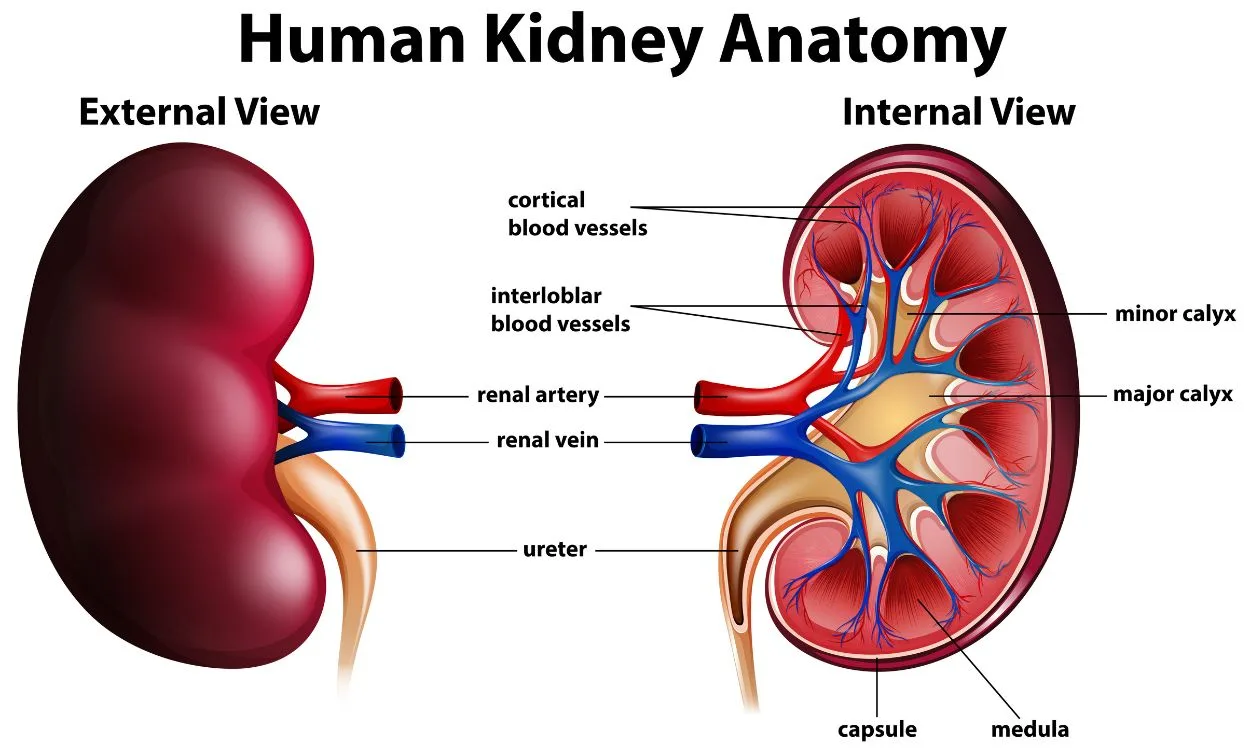
The Anatomy of the Kidneys
Before diving into the filtration process, it’s essential to understand the anatomy of the kidneys, as their structure is intricately linked to their function:
- Renal Cortex: The outer layer of the kidney, where blood is initially filtered.
- Renal Medulla: The inner part of the kidney, organized into pyramid-like structures called renal pyramids.
- Renal Pelvis: A funnel-shaped area at the center of the kidney that collects urine before it flows into the ureter.
- Nephrons: The functional units of the kidney, numbering in the millions per kidney. Each nephron consists of a renal corpuscle and renal tubules.
- Renal Corpuscle: Comprising the Bowman’s capsule and glomerulus, the renal corpuscle is where the initial filtration of blood occurs.
- Renal Tubules: These tubules include the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct. They play a crucial role in reabsorbing essential substances and further processing filtrate.
The Filtration Process
Renal filtration is a multi-step process that begins with blood entering the kidney via the renal artery. Here’s how it unfolds:
1. Glomerular Filtration
- Glomerulus: Within each nephron, the glomerulus is a dense network of capillaries surrounded by the Bowman’s capsule. Blood enters the glomerulus under high pressure due to the unique architecture of the afferent and efferent arterioles.
- Filtration: The high-pressure environment in the glomerulus forces small molecules like water, electrolytes, waste products (e.g., urea and creatinine), and some essential substances (e.g., glucose and amino acids) out of the bloodstream and into the Bowman’s capsule. This initial filtrate is known as “glomerular filtrate.”
2. Tubular Reabsorption
- Proximal Convoluted Tubule (PCT): As the glomerular filtrate moves into the PCT, many essential substances, such as glucose, amino acids, and electrolytes, are actively reabsorbed back into the bloodstream. Passive reabsorption of water also occurs here.
- Loop of Henle: This loop has a descending and ascending limb. It plays a pivotal role in reabsorbing water and electrolytes, primarily sodium and chloride ions. The descending limb is permeable to water, while the ascending limb is impermeable to water but actively transports ions.
- Distal Convoluted Tubule (DCT): Fine-tuning of electrolyte balance occurs in the DCT, under the influence of hormones like aldosterone and parathyroid hormone. It regulates the reabsorption of sodium, potassium, and calcium ions.
3. Tubular Secretion
- In this phase, the renal tubules actively transport substances (e.g., hydrogen ions and potassium ions) from the bloodstream into the tubular fluid. This secretion process helps in the elimination of excess substances and the maintenance of acid-base balance.
4. Collecting Duct
- The collecting ducts receive processed filtrate from multiple nephrons. Here, the final adjustments to water reabsorption are made, under the influence of antidiuretic hormone (ADH). ADH regulates the permeability of the collecting duct to water, conserving water when needed.
5. Excretion of Urine
- The remaining fluid, now called urine, exits the collecting duct and enters the renal pelvis, from where it flows into the ureter, then to the bladder, and ultimately out of the body.
Regulation of Renal Filtration
The process of renal filtration is under precise regulation to ensure that the body’s needs are met while maintaining homeostasis. Several hormones and feedback mechanisms control filtration and reabsorption rates:
- Renin-Angiotensin-Aldosterone System (RAAS): Regulates blood pressure and sodium balance.
- Antidiuretic Hormone (ADH): Controls water reabsorption in response to changes in blood osmolarity.
- Atrial Natriuretic Peptide (ANP): Acts to reduce blood volume and blood pressure.
- Parathyroid Hormone (PTH): Regulates calcium and phosphate balance.
Significance for Health
The kidneys’ ability to filter waste from the blood and maintain the body’s internal environment is vital for overall health. Dysfunction in renal filtration can lead to serious health issues, including kidney disease, hypertension, electrolyte imbalances, and fluid retention.
Conclusion
Renal filtration is a remarkable and complex process that exemplifies the kidney’s critical role in maintaining bodily homeostasis. From glomerular filtration to tubular reabsorption and secretion, the kidneys efficiently filter waste products, regulate electrolyte balance, and control blood pressure. Understanding this intricate process underscores the importance of kidney health and the significance of maintaining a balanced and hydrated lifestyle. The kidneys, through their relentless work, exemplify the elegance and precision of the human body’s physiological mechanisms.